Abstract
Introduction: Graft-versus-host disease (GVHD) remains a significant complication of allogeneic hematopoietic cell transplant (alloHCT), despite use of HLA-identical donors. Minor histocompatibility antigens presented to donor T-cells by recipient major histocompatibility complexes (MHCs) are central to GVHD pathophysiology, and prediction of GVHD occurrence in HLA-identical transplants remains problematic. Prior data show that informative HLA genotypes bind peptide epitopes with varying degrees of efficiency. Therefore, the cumulative peptide binding efficiency based on HLA-A, -B, and -C in HLA-identical transplants is estimable. We hypothesized that recipients with HLA-genotypes predicting lower cumulative peptide binding will experience lower rates of GVHD and higher rates of relapse following alloHCT.
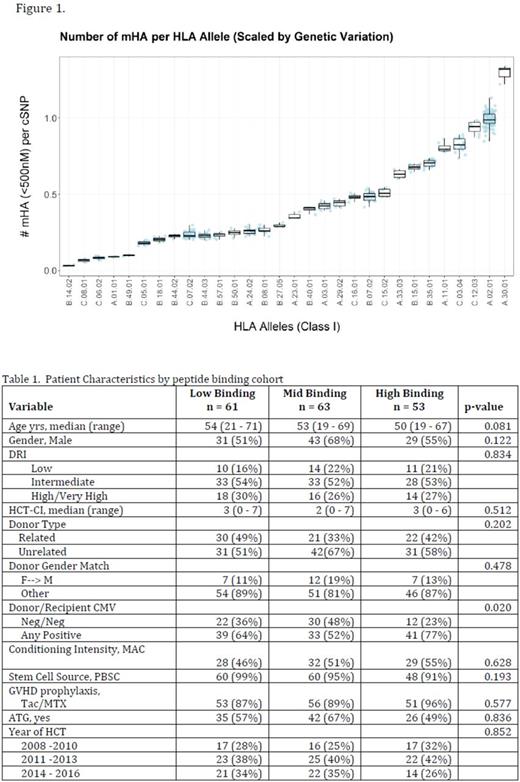
Methods: We retrospectively assessed 177 adult patients (median age 53 years, range 19-71) who received fully-matched alloHCT for hematologic malignancy between 01-01-2008 and 06-30-2016. All patients had a minimum of 4/6 informative HLA Class I alleles (Figure 1). Patients were grouped according to their cumulative peptide-binding fraction, measured as predicted peptide epitopes per SNP, into low-(LOW, n=61; median=0.3198, range 0.1730-0.3790), moderate-(MOD, n=63; median=0.4380, range 0.3802-0.5165), and high-(HI, n=53; median=0.5604, range 0.5248-0.7920) binding cohorts to compare transplant outcomes of survival, GVHD, and relapse.
Results: Table 1 shows patient, donor, and transplant characteristics by binding cohort. There were no differences between the groups with the exception that the moderate binding group had significantly more donor/recipient CMV seronegative pairs (p=0.02). The median follow-up for survivors was 42 months (5-109) and did not differ between groups [LOW: 34 mo (5-94) vs MOD: 37 mo (6-109) vs HI: 52 mo (7-103); p=0.459]. The cumulative incidence of Grade II - IV aGVHD by 100 days [LOW: 34% (95% confidence interval, CI) (23-50) vs MOD: 34% (24 - 48) vs HI: 25% (15-42); p=0.49]; moderate-severe cGVHD by 3 years [LOW: 30% (19-47) vs MOD: 19% (10-36) vs HI: 33% (23-48); p=0.31]; and relapse by 3 years [LOW: 32% (24-44) vs MOD: 40% (30-54) vs HI: 30% (19-46); p=0.45] did not differ between the binding cohorts. The 3-year overall survival by binding cohort was also similar [LOW 41% (27-54) vs MOD 53% (40-65%) vs HI 56% (41-69); p=0.25. In multivariable analysis, there was a decreased risk of aGVHD for patients receiving a NMA/RIC conditioning regimen [HR 0.36 (0.19-0.68); p=0.002] whereas male recipients with a female donor had a higher risk of aGVHD [HR 2.6 (1.33-5.09), p=0.005]. The use of ATG decreased the risk of chronic GVHD [HR 0.32 (0.15-0.65); p=0.002] but also increased the risk of death [HR 1.62 (1.02-2.56); p=0.04]. High/Very High DRI [HR 2.25 (1.0-5.04); p=0.05) increased relapse risk. Other variables examined, including the main effect of binding intensity as well as HCT-CI and age, did not significantly impact outcomes in our small patient population.
Conclusions: Discretizing HLA Class I peptide binding efficiency did not identify a difference in transplant outcomes. Further analysis incorporating informative HLA Class II binding efficiencies is underway. Due to limited patient numbers, we were unable to examine unrelated donors separately, where increased GVHD occurs, in part, due to higher quantities of minor histocompatibility antigens. Small differences in minor antigen number may not be associated with clinical outcomes. Instead, a subset of immunodominant minor histocompatibility antigens may drive GVHD development and relapse. Future experiments to determine the extent that immunodominant minor histocompatibility antigens are shared between recipients are necessary.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.